Creating a backbone around which to lose fat
Glucose is an indispensable metabolic fuel for the brain. For the reason that the brain is unable to synthesize glucose or store more than a few minutes supply as glycogen, it is critically dependent on a continuous supply of glucose from the circulation. "At normal (or elevated) arterial glucose concentrations, the rate of blood-to-brain glucose transport exceeds the rate of brain glucose metabolism. However, as arterial glucose levels fall below the physiological range, blood-to-brain glucose transport becomes limiting to brain glucose metabolism, and ultimately survival." -
Hypoglycemia in Diabetes, Philip E. Cryer, Diabetes Care 26:1902-1912, 2003
So what happens at various blood glucose levels?
For practical purposes we can say that the body desires to maintain a
stable glucose level in blood plasma of around 90 ng/dL. Blood glucose levels above that threshold are viewed as excess energy and this engenders a storage response via the pancreatic secretion of insulin. The hormone insulin removes glucose from blood plasma until levels return to 90ng/dL at which point insulin ceases to be active.
Below that insulin triggering blood glucose threshold of
90ng/dL, down to about 70ng/dL, there is insufficient circulating energy and therefore the hormone glucagon is released to catabolize stored energy and make it available to the brain and body. Physical activity or energy demanding activity without the presence of circulating glucose or concurrent intake of food requires stored energy. Activity is the catalyst that drives the blood glucose level below 90ng/dL.
Below 70ng/dL of glucose in blood plasma the body becomes concerned and because the brain is a critical organ and needs glucose, this threshold is considered critical. The hormone epinephrine (adrenaline) is released at this stage in order to trigger a quick release of stored energy to get blood glucose levels back to normal.
The body when it is in this emergency state will burn anything for fuel and muscle can be catabolized. It is best to avoid this state.
When you diet you can not lose fat in the presence of the hormone insulin. You want to have the hormone glucagon active and this requires that your blood glucose levels be between
70ng/dL and 90ng/dL. Glucagon acts to free up stored energy by signaling the adipocytes to activate Hormone-sensitive lipase which converts triglycerides into free fatty acids.
Hormone-sensitive lipase is a vital component of fat mobilization and is a positively active force in the presence of glucagon and inhibited in the presence of insulin.
Fatty acids have very low solubility in the blood however serum albumin, binds free fatty acids, and thereby increases their effective solubility by a factor of about 1000. Serum albumin transports fatty acids to organs such as muscle and liver for oxidation and this happens when blood sugar is low.
So what is the minimal amount of glucose needed to trigger insulin & why again is insulin bad?
From the textbook
Biochemical and Physiological Aspects of Human Nutrition, Stipanuk et al. ed. 2000
Insulin ...is secreted in response to changes in circulating glucose; a change of as little as 2mg/100ml of plasma can be detected by the pancreas. Insulin release can also be stimulated in response to certain amino acids in the circulation. Other important signals for insulin secretion include gut hormones and nervous stimulation. - p395
In adipose tissue insulin increases fatty acid uptake and triacylglycerol storage via increases in lipoprotein lipase activity, and at the same time decreases lipolysis by decreasing hormone-sensitive lipase activity. The latter may be one of insulin's strongest actions because it occurs at very low insulin levels and effectively lowers the levels of free fatty acids in the circulation thereby decreasing there utilization as fuel. - p396
Is there way to minimize glucose's influence?
Again from the textbook
Biochemical and Physiological Aspects of Human Nutrition, Stipanuk et al. ed. 2000
Soluable viscous polysaccharides [certain fibers] can delay and even interfere with the absorption of nutrients...
Positive benefits of delayed nutrient absorption include an improvement of glucose tolerance and a lowering of serum cholesterol levels. Delayed absorption of carbohydrates results in a lower postprandial (following a meal) glucose level. In general the more viscous the fiber the greater the effect on blood glucose. This is similar to the effect seen with eating several small meals rather than one large meal. When glucose is absorbed in small amounts over an extended period, such as seen with viscous fibers, the insulin response is attenuated (Pick, et al. (1996) Oat bran concentrate bread products improve long term control of diabetes: A pilot study J. Am Diet Assoc 96:1254-1261)
...
Viscosity of the polysaccharides and their ability to form gels in the stomach appear to slow gastric emptying. This in turn results in a more uniform presentation of the meal to the small intestine for absorption. [Poorly soluble fibers that do not form gels such as wheat and cellulose have little effect...unlike those that do which include guar gum, pectin, psyllium, oat bran.] - p146. 147
A Practical Experiment
For two days I used my glucose monitor to check my blood glucose after ingestion of coffee.
- Black coffee w/ no additives = zero rise in glucose
- Black coffee w/ Stevia = a 2 point rise in glucose
- Black coffee w/ Splenda = a 5 - 8 point rise in glucose.
- Coffee w/ Splenda & generic Coffee Mate creamer = 15+ point rise in glucose
- Coffee w/ Splenda & 2% Lactose free Milk = 17+ point rise in glucose
So for me the caffeine in a cup of coffee does not effect blood glucose BUT the additives sure as heck do!
How do you reduce the rise in blood glucose w/ these additives (besides the obvious)? ....
add FIBER.
So ingesting 2 grams of
Psyllium Husk powder just prior to drinking Coffee w/ Splenda & Coffee Mate creamer resulted in only a 4 point rise in blood glucose.
WOW!
So how does Growth Hormone fit in to all of this?
First recognize that there will be periods of time post meal where blood glucose and thus insulin will be elevated. There is no fat loss during this time and Growth Hormone will not be effective during these periods.
With this recognition it makes sense to reduce the amplitude and area under the curve (in graph-type language) of insulin spikes. Meals should be constructed with both the glycemic index of foods in mind and the total glycemic load of the meal. Fiber should be used to reduce blood glucose levels.
With this recognition it makes sense to maximize the time period when glucagon is active. That requires insulin to return to baseline quickly after a meal and a sufficient period of time between meals to allow glucagon to have an effective impact. Activity between meals as well as the presence of GH will have positive impacts on fat loss.
The reason it is necessary to write about everything in this post is so that you understand how easy it is to waste Growth Hormones fat loss potential and what one must do to maximize GH's fat loss power.
Too often someone will use GH and admit that their diet wasn't very good. That negates much of GH's positive impact on fat loss.
I also wanted to put GH into a proper context which sadly is often lacking in people who hope for better body attainment. The things I have barely touched on are of utmost importance and make up the backbone of a sound fat loss protocol.
GH can be a very useful adjunct to a properly constructed protocol which focuses on food intake with proper hormonal impact and sustained activity level.
Use of GH
From other posts we understand that GH has a dual role to play in a diet. It can increase the rate of fat loss and it can help inhibit the breakdown of muscle. So you want to administer GH in smaller amounts, you want to have off periods (i.e. time when GH is not active) so that the intracellular pathways can reset and you want to maximize the frequency of administration.
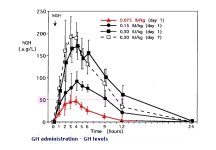
So we need to understand the impact of GH dose on levels of GH in plasma to set a schedule. We can extrapolate from the chart from the GH study posted above. Assuming a linear relationship (since 7.5ius were active for 12 hours & 15ius for 24 hours) we can assume that a dose of 2ius of synthetic GH administration will elevate GH in plasma for 3.2 hours.
If we need about 4 hours off (we can probably round down to 3.8 hours) we can dose 2ius of GH every 7 hours. For ease of fitting a dosing schedule into our lives we can round up to 8 hours and say that we can dose 2ius three times a day spaced out by 7-8 hours.
Since GH isn't effective for fat loss in the presence of insulin we probably want the meals that have the biggest impact on blood glucose and thus insulin to be ingested during the time GH is not active. After that meal is digested and insulin rises and then falls back to 90ng/dL we can administer GH and be confident it will have a positive impact on our overall fat loss protocol.