Protein Metabolism - The complementary role of various hormones in inducing Anabolism
Too many people have very little idea how the following factors work together in increasing protein synthesis and preventing protein breakdown. If they truly understood these things would they give up seeking THE magic bullet? I doubt it... Would they stop seeking out self-proclaimed gurus who in my opinion fail miserably in understanding these things themselves.
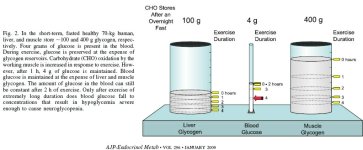
- Insulin
- Growth Hormone
- Amino Acid Pool
- Exercise
- Blood Flow
- IGF-1
- IGF-1/IGFBP-3
- Androgens
- Thyroid Hormones
What follows are basically my notes structured in such a way as to be highly readable, massively informative and well referenced for further research should someone be so inclined.
I didn't really intend to post this for public consumption so forgive the format. I ask that you not cut and paste this post onto other forums. Basically it is here for anyone who reads this thread and no one else.
The following post was derived both generally and specifically from the following studies. Additional studies are provided as references for selective material herein.
An abundant supply of amino acids enhances the metabolic effect of exercise on muscle protein, Gianni Biolo, Am. J. Physiol. 273 (Endocrinol. Metab. 36): El22-E129, 1997.
Acute Growth Hormone Effects on Amino Acid and Lipid Metabolism, K. C. Copeland, Journal of Clinical Endocrinology and Metabolism Vol. 78, No. 5 1994
Effects of Insulin-Like Growth Factor-1/Binding Protein-3 Complex on Muscle Atrophy in Rats, Martin M. Zdanowicz, 2003 by the Society for Experimental Biology and Medicine
Hormonal regulation of human protein metabolism, Pierpaolo De Feo, Eur J Endocrinol 1996:135:7-18
Physiologic Hyperinsulinemia Stimulates Protein Synthesis and Enhances Transport of Selected Amino Acids in Human Skeletal Muscle, Gianni Biolo, J. Clin. Invest. vol. 95, 811 - 819
Skeletal muscle protein anabolic response to resistance exercise and essential amino acids is delayed with aging, Micah J. Drummond, J Appl Physiol 104: 1452-1461, 2008
Compartmental model of leucine kinetics in humans, Claudio Cobelli, Am. J. Physiol. 261 (Endocrinol. Metab. 24): E539-E550, 1991
Dose-response curves of effects of insulin on leucine kinetics in humans, Paolo Tessari, Am. J. Physiol. 251 (Endocrinol. Metab. 14): E334-E342, 1986.
Growth hormone decreases muscle glutamine production and stimulates protein synthesis in hypercatabolic patients, Gianni Biolo, Am J Physiol Endocrinol Metab 279:323-332, 2000
Increased rates of muscle protein turnover and amino acid transport after resistance exercise in humans, Gianni Biolo, Am. J. Physiol. 268 (Endocrinol. Metab. 31): E514-E520, 1995.
Insulin action on protein metabolism in acromegalic patients, Alberto Battezzati, Am J Physiol Endocrinol Metab 284:823-829, 2003
Leucine and phenylalanine kinetics during mixed meal ingestion a multiple tracer approach, Gianni Biolo, Am. J. Physiol. 262 (Endocrinol. Metab. 25): E455-E463,1992.
Protein synthesis and breakdown in skin and muscle a leg model of amino acid kinetics, Gianni Biolo, Am. J. Physiol. 267 (Endocrinol. Metab. 30): E467-E474, 1994.
Transmembrane transport and intracellular kinetics of amino acids in human skeletal muscle, Gianni Biolo, Am. J. Physiol. 268 (Endocrinol. Metab. 31): E75-E84, 1995.
Insulin
There is indirect evidence that post-prandial [after a meal] hyperinsulinemia induces protein anabolism, other than through the suppression of whole-body proteolysis [i.e. protein breakdown/ catabolism], also by facilitating the incorporation of dietary amino acids into new proteins. In fact, when post-prandial hyperinsulinemia and hyperaminoacidemia [high insulin & high amino acids] are reproduced in normal subjects by a combined intravenous infusion of insulin and amino acids, the estimates of whole-body protein synthesis increase more than after amino acids alone (20).
[Insulin + Amino Acids = greater increase in entire body protein synthesis]
The stimulatory effect of hyperinsulinemia on whole-body protein synthesis cannot be demonstrated when insulin alone is infused (20-25). In this case, by reducing the rate of protein breakdown, hyperinsulinemia decreased the intracellular concentrations of most amino acids (26), limiting their utilization for protein synthesis (27).
[In other words the store of amino acids (often called the intracellular amino acid pool) is replenished in two ways. One by eating/ingestion of protein & the other by the breakdown of protein in muscle (i.e. protein degradation). This latter, protein degradation reduces protein to its constituent parts (amino acids) which will be transported outside the cell & either be further removed or remain in the amino acid pool (which resides between muscle cells) and is available for reuse in muscle for the next round of transport into muscle & new protein synthesis. Insulin reduces protein breakdown so the amino acid pools are not replenished.]
Branched-chain amino acids are particularly sensitive to hyperinsulinemia (28) and it has been shown the insulin-induced suppression of plasma isoleucine concentration (29), i.e. of a single essential amino acid, is sufficient to decrease wholebody protein synthesis.
[So in essence protein synthesis requires all the essential amino acids. If one is missing no protein synthesis will occur.]
The results of recent studies demonstrate that the effects of insulin on whole-body protein kinetics represent the mean results of differential effects of the hormone on the rates of protein breakdown and synthesis of individual proteins. For instance, despite the rate of whole-body proteolysis being decreased by insulin (20-25), the rate of muscle protein proteolysis is not affected by local hyperinsulinemia (30). Such a differential effect can be explained by the fact that insulin decreases the proteolytic activity of lysosomes but does not control the ubiquitin system (31) that is responsible for the bulk of muscle proteolysis (31).
[So insulin decreases protein breakdown/degradation throughout the entire body but does not inhibit protein breakdown specifically in muscle.]
References:
20 - Castellino P, Luzi L, Simonson DC. Haymond M. DeFronzo RA. Effect of insulin and plasma amino acid concentrations of leucine metabolism in man: role of substrate availability on estimates of whole body protein synthesis. J Clin Invest 1987: 80:1784-9 3
21 - Fukagawa NK. Minaker KL. Rowe JW. Goodman MN. Matthews DE. Bier DM, et al. Insulin-mediated reduction of whole body protein breakdown: dose-response effects on leucine metabo¬ lism in postabsorptive men. J Clin Invest 1985:76:2306-11
22 - Tessari P, Trevisan R, Inchiostro S, Biolo G, Nosadini R, De Kreutzenberg SV, et al. Dose-response curves of effects of insulin on leucine kinetics in humans. Am J Physiol 1986;251:E334-42
23 - Tessari P. Nosadini R. Trevisan R. De Kreutzenberg SV. Inchiostro S. Duner E. et al. Defective suppression by insulin of leucine-carbon appearance and oxidation in type 1, insulin dependent diabets mellitus: evidence for insulin resistance involving glucose amino acid metabolism. J Clin Invest 1986:77:1797-804
24 - Luzi L, Castellino P. Simonson DC, Petrides AS, DeFronzo RA. Leucine metabolism in IDDM: role of insulin and substrate availability. Diabetes 1990:39:38-48
25 - De Feo P. Volpi E, Lucidi P, Cruciani G. Reboldi G. Siepi D, et al. Physiological increments in plasma insulin concentrations have selective and different effects on synthesis of hepatic proteins in normal humans. Diabetes 1993:42:995-1002
26 - Alvestrand A, DeFronzo RA, Smith D, Wahren J. Influence of hyperinsulinaemia on intracellular amino acid levels and amino acid exchange across splanchnic and leg tissues in uraemia. Clin Sci 1988;74:155-63
27 - De Feo P. Haymond MW. Effect of insulin on protein metabolism in humans: methodological and interpretative questions. Diab Nutr Metab 1991:4:241-9
28 - Fukagawa NK. Minaker KL. Young VR. Rowe JW. Insulin dosedependent reductions in plasma amino acids in man. Am J Physiol 1986;250:E13-7
29 - Lecavalier L, De Feo P. Haymond MW. Isolated hypoisoleucinemia impairs whole body but not hepatic protein synthesis in humans. Am J Physiol 1991;261:E578-86
30. Biolo G, Declan Fleming RY. Wolfe RR. Physiologic hyper¬ insulinemia stimulates protein synthesis and enhances trans¬ port of selected amino acids in human skeletal muscle. J Clin Invest 1995:95:811-9
Insulin increases the amount of protein deposited in muscle by directly increasing the rate of protein synthesis (40-60% as measured by lysine & phenylalanine dissapearance from intracellular pools). Insulin does not increase (or regulate) transmember amino acid transport. Therefore transportation of amino acids is not a primary mediator of insulin anabolic actions in muscle.
[So Insulin's primary modes of action are reduction of whole-body protein breakdown as discussed already & in muscle an increase in the rate of protein synthesis. Now it draws on the intracellular pool of amino acids to effect this increased synthesis. It is possible to run out of amino acids from that pool. Insulin can suck the reservoir dry so to speak.
In addition insulin in general (there is an exception) does not increase the rate of transportation of amino acids across the cell membrane into the cell. That remains normal. But the benefit of insulin in muscle is that it increases protein synthesis. However other things are needed besides insulin to effect anabolism.]
Insulin draws on an existing intracellular pool of amino acids. When amino acid concentrations are maintained at levels higher than normal during systemic insulin administration insulin increased muscle protein synthesis (40).
[So anabolism occurs when both insulin increased protein synthesis occurs and amino acid levels are maintained higher then normal. The primary way to effect this is to increase amino acid/protein ingestion.]
40. - Bennett, W. M., A. A. Connacher, C. M. Scringeour, R. T. Jung, and M. J. Rennie. 1990. Euglycemic hyperinsulinemia augments amino acid uptake by human leg tissues during hyperaminoacidemia. Am. J. PhysioL 259:E185-E194
Insulin does not significantly modify protein breakdown in muscle. It has been shown that, during adequate amino acid supply, the most important degradative system in muscle is an ATP-independent system that requires the presence of a specialized protein, termed ubiquitin. This system is not sensitive to insulin. Concerning protein breakdown Insulin apparently plays a role only in the regulation of the lysosome activity. These intracellular organelles are not involved in the myofibrillar protein degradation in normal conditions, but only in the presence of low insulin levels or decreased amino acid availability).
[So again insulin will increase protein synthesis in muscle but will not inhibit protein breakdown. So in general anabolism will occur if more protein synthesis then protein breakdown occurs.]
Following protein degradation, the amino acids from the degradation event are either transported outward (or in the case of leucine oxidized) or are redirected back into protein synthesis. Phenylalanine & leucine have been shown to be redirected back into protein synthesis while lysine may not.
Insulin induces hyperpolarization in the skeletal muscle cells by directly activating the sodium ion (Na+) and potassium ion (K+) -ATPase pump. Those amino acids which are strongly "attracted" to the electrochemical characteristics of the cell membrane are more readily taken up into muscle from the intracellular pool of amino acids. Alanine & lysine are two amino acids that have this attraction and are more readily drawn into muscle by insulin.
[When protein in muscle is broken down and its constituents removed back to the amino acid pool, those amino acids may be removed from muscle pools entirely, may be reused for new synthesis or for some amino acids oxidized or used for energy. It would not benefit anabolism to lose the important amino acid leucine to oxidation.
Insulin which in general doesn't increase transport of amino acids from pool into cells, does so for a few amino acids which use NA+ & K+ channels, namely alanine & lysine.]
The branched-chain amino acids (leucine, valine, and isoleucine) and the aromatic (phenylalanine and tyrosine) are preferably transported through system L . This sodium-independent system is unable to generate high transmembrane gradients for its substrates. It has been shown that the kinetic characteristics of system L are not influenced by insulin.
[So insulin which has no effect on this mode of transport does not increase the uptake of some very important amino acids.]
Blood flow has been found to increase local amino acid delivery to muscle and secondarily increase amino acid transport. This effect may be responsible for increase in leucine uptake.
[This is an extremely important way in which amino acids are drawn to muscle and into cells. Time and again the important amino acid leucine has been shown to make its way into cells via increase in blood flow.]
Alanine synthesis (which is a function of pyruvate) also increases in the presence of insulin because insulin increases glucose uptake & intracellular pyruvate in muscle.
[Certain amino acids can be synthesized from the breakdown of other amino acids. Alanine is one of them. Alanine is often used for energy and so protein synthesis rate or anabolism may depend on the availability of alanine not yet oxidized. The fact that insulin increases alanine synthesis is a desirable effect.]
The anabolic effect of insulin on muscle may have become self-limited because of an intracellular depletion of precursor amino acids for protein synthesis, unless amino acid transport is independently stimulated by other factors, i.e., amino acid administration.
[Again an external source of amino acids is needed to make insulin anabolic in muscle.]
31. Kettlehut IC. Wing SS. Goldberg AL. Endocrine regulation of protein breakdown in skeletal muscle. Diab Metab Rev 1988;4:751-72
---
Growth Hormone
See:
Post #777 - What does GH contribute to anabolism besides creating IGF-1?
Growth hormone promotes protein anabolism with mechanisms different from insulin. It does not affect the rates of whole-body proteolysis but decreases those of amino acid oxidation (51, 52). The sparing effect on amino acid oxidation results in a greater rate of their incorporation into proteins (51-53), with a net protein anabolic effect.
51. Horber FF. Haymond MW. Human growth hormone prevents the protein catabolic side effects of prednisone in humans. J Clin Invest 1990:86:265-72
52. Copeland KC. Nair KS. Acute growth hormone effects on amino acid and lipid metabolism. J Clin Endocrinol Metab 1994: 78:1040-7
53. Yarasheski KE. Campbell JA. Smith K, Rennie MJ, Holloszy JO, Bier DM. Effect of growth hormone and resistance exercise on muscle growth in young men. Am J Physiol 1992;262:E261-7
[So Growth Hormone decreases amino acid oxidation (or break down for energy). This should have the effect of preserving key amino acids in that very important amino acid pool. This means that muscle protein synthesis or even increased muscle protein synthesis induced by insulin will be more prolonged because there will be a larger pool of raw material (aminos) to draw from.]
---
Growth hormone decreases muscle glutamine production
In agreement with previous observations in animals (20, 23), this study shows that rhGH infusion in traumatized patients accelerates the rates of transmembrane transport of the essential amino acids leucine and phenylalanine. This effect was independent of changes of leg blood flow and arterial amino acid concentrations. This rhGH-mediated increased ability of transmembrane systems to transport essential amino acids confirms previous observations in vitro (20, 23) and represents a novel observation in vivo.
[So while insulin increases transport of a few aminos (alanine & lysine), GH increases amino acid transport for leucine and phenylalanine. This would mean that GH would increase transport of the other aromatic amino acid tyrosine and the other branch-chain amino acids valine and isolecine]
Besides stimulating protein synthesis, growth hormone suppressed the rate of catabolism of the branched-chain amino acids leucine, isoleucine, and valine. This effect has been reported by several other authors using isotopic tracers of leucine at the whole body level (8, 12).
[So growth hormone unlike insulin suppresses the breakdown and loss of branch-chain amino acids & probably all amino acids. Thus GH provides more raw material for insulin-induced higher rate of protein synthesis.]
Glutamine and alanine constitute the major carriers of nitrogen among body tissues (2).In skeletal muscle, these amino acids are constantly being synthesized and released into the bloodstream (2). In severe trauma, alanine release from muscle is greatly accelerated, whereas glutamine release was found to be increased or unchanged (5). Our results indicate that rhGH administration selectively decreases the rates of synthesis and release of glutamine, whereas alanine synthesis did not change during the hormone administration.
[Growth hormone has a negative effect on glutamine synthesis.]
In our patients, whole body skeletal muscle released 19 g of glutamine per day into the bloodstream before rhGH administration. After rhGH administration, glutamine release from skeletal muscle decreased by 50%, whereas at the whole body level, glutamine clearance tended to decrease by 15%.
[So glutamine which is very important to the immune system & is urgently needed in times or severe trauma is not really made available. This in part may be the reason why death occurs in critically ill patients given GH.]
The obvious solution for this potential side effect of growth hormone treatment in critically ill patients is to simultaneously administer exogenous glutamine to offset the decreased availability of the endogenous amino acid.
[This also is a lesson for those seeking muscle anabolism while using GH. Less glutamine is synthesized and thus available in the presence of GH. Thus supplementation with glutamine should increase the potential for anabolism.]
---
Amino Acid Pool
From a dynamic point of view, such muscle hypertrophy results from changes in the rates of protein synthesis and/or breakdown. In addition, an acceleration of the rates of amino acid transport into muscle cells may contribute to muscle anabolism by increasing amino acid availability for protein synthesis. Studies suggest that muscle protein accretion occurs in the recovery phase after exercise rather than during the actual exercise period. The leucine tracer incorporation technique has shown that the rate of muscle protein synthesis in humans is increased after exercise (7) and remains elevated for > 24 h (7).
In these studies, muscle protein breakdown was not ddirectly measured. However, the increase in protein synthesis was so large that if it were not accompanied by a concomitant increment in protein breakdown, exercise training would result in a greater increase in muscle size than actually occurs.
7. Chesley, A., J. D. MacDougall, M. A. Tarnopolsky, S. A. Atkinson, and K. Smith. Changes in human muscle protein synthesis after resistance exercise. J. AppZ. Physiol. 73: 1383- 1388,1992.
Exercise
We found that, after exercise, the rates of muscle protein turnover and amino acid transport were increased. Protein synthesis and breakdown increased simultaneously but to a different extent. Synthesis increased by - lOO%, whereas breakdown increased by only - 50%. Consequently, protein balance (synthesis minus breakdown) improved after exercise (becoming not significantly different from zero) but did not shift to a positive value. These results suggest that physical exercise can restrain net muscle protein catabolism but does not directly promote net protein deposition in the postabsorptive state. Thus exercise probably needs to interact with other factors, such as feeding, to promote muscle anabolism.
[Although this paragraph is not completely clear, having read the studies I can say that the take home message is that exercise reduces catabolism. Exercise increase both breakdown & synthesis of protein but that exercise alone will not tilt things toward anabolism. Amino acid availability is required.]
The notion that increased amino acid availability can directly regulate protein synthesis is further supported by the fact that the rate of synthesis was enhanced during amino acid infusion or in catabolic patients, in whom a large primary increase of breakdown occurs. In the present study therefore the acceleration of protein breakdown and amino acid transport may have contributed to the increase in protein synthesis. Because of the increase in amino acid transport, the changes in protein degradation have been more than offset by the increased rate of synthesis.
We found that, after exercise, the absolute rate of protein breakdown was accelerated. This catabolic response almost counteracted the increase in protein synthesis.
[So exercise + amino acids = anabolism]
Our study suggests that this mechanism may also be important for amino acid and protein metabolism. Thus physical exercise may not have a direct regulatory effect on the membrane transport systems, but its effect may be due to the increased amino acid delivery to muscle tissue secondary to the increased blood flow.
Anabolism vs Catabolism
The intracellular availability of amino acids may not be the sole acute regulator of muscle protein synthesis, inasmuch as hormones and other factors may have direct effects. Nonetheless it seems clear that the rates of breakdown and inward amino acid transport are important factors. The importance of variations in inward transport can be appreciated when the difference between the anabolic response to exercise is compared with the catabolic response to critical illness. In both circumstances, the rate of breakdown is increased, but in the case of critical illness, inward transport is relatively impaired, rather than stimulated. As a consequence, muscle synthesis is not stimulated to the same extent as breakdown, with net catabolism resulting. Thus the increase in inward transport after exercise appears to be an important response that enables synthesis to increase to a greater extent than breakdown.
Side Note (skin more important then muscle)
Thus the stability of muscle mass throughout the day is maintained by alternating phases of catabolism during fasting and anabolism after feeding. This process is necessary to supply liver and gut with amino acids for protein synthesis in the fasting state. Our data suggest that the same mechanism is not involved in the skin, because, after - 20 h of fasting, we did not observe any net loss of essential amino acids from this tissue. From these results, it appears that maintenance of skin mass is a high metabolic priority, and this may occur, at least in part, at the expense of muscle tissue.
---
Blood flow
Over the last decade, evidence has accumulated supporting the hypothesis that blood flow is a major regulator of glucose uptake in skeletal muscle (1).
1. Baron, A. D., H. Steinberg, G. Brechtel, and A. Johnson. Skeletal muscle blood flow independently modulates insulinmediated glucose uptake. Am. J. Physiol. 266 (Endocrinol. Metab. 29): E248-E253,1994.
The results of our study suggest that variations in blood flow may also affect muscle protein metabolism by increasing transport of free amino acids into cells, which in turn stimulates protein synthesis. This notion is supported by the high correlation between blood flow and FSR.
In summary, the results of our study demonstrate that net protein synthesis during amino acid administration can be doubled by previous performance of heavy resistance exercise. Moreover, the data suggest a link between the stimulation of protein synthesis after exercise and an acceleration in amino acid transport. The greater rate of transport after exercise may be due to the increase in blood flow.
An abundant supply of amino acids enhances the metabolic effect of exercise on muscle protein , Gianni Biolo, Am. J. Physiol. 273 (Endocrinol. Metab. 36): El22-E129, 1997.
[So Exercise + increased bloodflow + amino acids = increased amino acid transport. Of course this leads to the understanding that aminos need to be in the blood prior to the increased blood flow of exercise.]
----
IGF-1
The data available in humans indicate that IGF-I has a mechanism of action similar to insulin on protein metabolism (62-65) because IGF-I administration also reduces the rates of whole-body protein breakdown and synthesis. When compared on a molar basis, the action of IGF-I is ~ 14 times less potent than that of insulin (65),
IGF-I might affect protein metabolism only in selected tissues through a paracrine action on whether IGF-I, due to its longer half-life could influence whole-body protein metabolism when plasma GH concentrations decline; and the role played by IGF-I binding proteins in the modulation of the endocrine action of IGF-I on protein metabolism needs to be established.
62. Turkalj I. Keller U. Ninnis R, Vosmeer S, Stauffacher W. Effect of increasing doses of recombinant human insulin-like growth factor I on glucose, lipid and leucine metabolism in man. J Clin Endocrinol Metab 1992;75:1186-91
63. Mauras . Horber FF, Haymond MW. Low dose recombinant human insulin-like growth factor-1 fails to affect protein anabolism but inhibits islet cell secretion in humans. J Clin Endocrinol Metab 1992;75:1192-7
64. Elhay D. McAloon-Dyke M. Fukagawa NK, Sclater AL, Wong GA. Shannon RP. et al. Effects of recombinant human IGF-1 on glucose and leucine kinetics in men. Am J Physiol 1993:265: E831-8
65. Giordano M, Castellino P. Carrol CA, DeFronzo RA. Comparison of the effects of human recombinant insulin-like growth factor 1 and insulin on plasma amino acid concentrations and leucine kinetics in humans. Diabetologia 1995:38: 732-8
---
IGF-1/IGF-1 Binding Protein 3 complex
The major beneficial effect of IGF-1/BP3 in this study appeared to be reduced muscle proteolysis. IGF-1/BP3 significantly reduced net protein degradation rates in muscles from HLS rats. Preservation of muscle weight and protein content paralleled this reduced muscle proteolysis. In a previous study with highly catabolic muscle from dystrophic hamsters, we reported a 27% decrease in muscle protein degradation rates with rhIGF-1 (29); here with IGF-1/BP3, we report a near 40% decrease. A key component of muscle proteolytic pathways, namely calpain-mediated myofibrillar degradation, was also reduced in rhIGF-1-treated dystrophic mice (30)
Effects of Insulin-Like Growth Factor-1/Binding Protein-3 Complex on Muscle Atrophy in Rats Martin M. Zdanowicz, Experimental Biology and Medicine 228:891-897 (2003)
[So there is an action that GH alone nor insulin effects, namely the reduction in protein degradation/breakdown in muscle. Of course GH increases the amount of IGF-1/IGF-1 Binding Protein 3 complex.]
---
In humans, IGF-I administration promoted protein anabolism both by stimulating protein synthesis and by inhibiting protein degradation both in muscle and at the whole body level (10, 11).
10. Elahi D, McAloon-Dyke M, Fukagawa NK, Sclater AL, Wong GA, Shannon RP, Minaker KL, Miles JM, Rubenstein AH, Vandepol CJ, Guler H-P, Good WR, Seaman JJ, and Wolfe RR. Effects of recombinant human IGF-I on glucose and leucine kinetics in men. Am J Physiol Endocrinol Metab 265: E831–E838, 1993.
11. Fryburg DA. Insulin-like growth factor I exerts growth hormone- and insulin-like actions on human muscle protein metabolism. Am J Physiol Endocrinol Metab 267: E331–E336, 1994.
[So IGF-1 administration both stimulates protein synthesis and inhibits protein degradation in muscle & the entire body. However the reduction in protein degradation in muscle is unique to this hormone as this is not a benefit of GH's sole actions, of insulin's actions or of androgen action.]
---
Androgens
Pharmacological doses of androgens increase lean body mass in normal men (77) and muscle sized in trained athletes (78). The mechanisms responsible for the anabolic effects of testosterone have been explained by Griggs et al. (79). In a group of healthy volunteers, a 12-week administration of a pharmacological dose of testosterone enanthate increased mixed muscle protein synthesis (muscle biopsy during the infusion of labeled leucine) by 27% did not significantly affect leucine estimates of the whole-body protein breakdown...
...androgens promote protein anabolism by sparing amino acids from oxidation and increasing their incorporation into proteins, especially muscle proteins.
Thus, part of the effects attributed to androgens, namely the suppression of leucine oxidation (51, 52) and the stimulation of whole-body (51-53) and muscle (57- 59) protein synthesis, might be mediated by GH.
[So androgens supress amino acid oxidation and increase protein synthesis ...either alone or as a synergistic or complementary action of GH.]
---
Thyroid hormones (catabolic NOT anabolic)
In contrast, both rates of whole-body protein breakdown and synthesis are increased by the administration of T3 and T4 to normal subjects (110). Under these circumstances net protein catabolism occurs because the stimulation of protein synthesis is overcome by a greater stimulation of amino acid oxidation (110).
110. Tauveron I, Charrier S, Champredon C, Bonnet Y, Berry C, Bayle G, et al. Response of leucine metabolism to hyperinsulinemia under amino acid replacement in experimental hyperthyroidism. Am J Physiol 1995;269:E499-507
[Thyroid hormones are catabolic because they stimulate breakdown to a greater extent then synthesis.]
The data on the role played by normal thyroid hormone concentration in the physiological regulation of everyday protein metabolism in normal humans are very limited. In growing rats it has been suggested that thyroid hormones contribute to the increase in protein synthesis induced by meal absorption (113). This does not appear to be the case in humans, according to the evidence that meal-induced changes in protein kinetics occur in the absence of significant changes in the plasma concentrations of T3 and T4 (114).
113. Jepson MM, Bates PC, Millward DJ. The role of insulin and thyroid hormones in the regulation of msucle growth and protein turnover in response to dietary protein. Br J Nutr 1988;59:397-415
114. Pacy PJ, Price GM, Halliday D, Quevedo MR, Millward DJ. Nitrogen homeostasis in man: the diurnal responses of protein synthesis and degradation and amino acid oxidation to diets with increasing protein intakes. Clin Sci 1994:86:103-18
[Thyroid hormones do not appear to contribute to protein synthesis following meals in humans. In rats yes... In other words these hormones in normal humans do not add to the protein synthesis that meals induce.]
Basal concentrations of thyroid hormones have differential effects on individual protein kinetics and they play a role in the physiological regulation of protein metabolism of selectively modulating the synthetic or the catabolic rates of target proteins.
[Base levels of thyroid hormones play a general role in modulating both catabolism and synthesis of proteins. Other then restroing abnormalities there doesn't appear to be predictable benefit to manipulating thyroid hormone levels if anabolism is the goal.]
---
Catabolism
Cortisol, Glucagon, Thyroid hormones
Thus, whole-body and muscle protein catabolism induced by triple hormonal infusions appear to be mediated by a similar mechanism. The hormones, through the stimulation of protein breakdown, increase the intracellular availability of amino acids; the net catabolic effect results from the fact that hormonal action promotes the oxidative disposal of these amino acids more than their utilization for the synthesis of new proteins.
[These hormones, especially if they are present together promote protein breakdown and rather then making the amino acid pool available for resynthesis, they increase loss by stimulating oxidation.]